[heading centered=”yes” margin_bottom=”no”]Family History and Glaucoma[/heading]
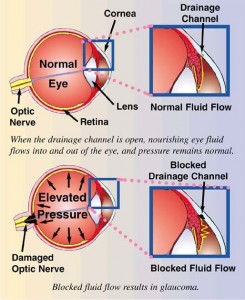
According to a study reported at the World Glaucoma Congress, the most efficient way to detect Primary Open-Angle Glaucoma (POAG), which is the most common form of glaucoma, is by knowing the medical history of close relatives with the disease. If you have a parent, sibling or child with POAG you have a greater than 25% chance of developing the disease. Others at risk include African Americans over 40, and anyone over 60, especially Mexican Americans. The earlier POAG is detected, the better the prognosis for retaining vision throughout one’s life. POAG occurs when the fluid that nourishes the eye cannot drain properly and the resulting increased pressure inside the eye damages the optic nerve. This is painless and not visually noticeable at first, but will lead to vision loss and blindness if left untreated. Increased pressure in the eye isn’t a sure sign of POAG, but it is a sign of increased risk for the disease. To read more about glaucoma click here.
Early diagnosis is of utmost importance. Dr. Griffith examines different parts of your eye to determine if you have or are at risk for developing POAG. Detection and diagnosis relies on tests for pressure within the eye (Tonometry), corneal thickness (Pachymetry) and observation of the optic nerve (Ophthalmoscopy),  quantification of the retinal nerve fiber layer (Optical Coherence Tomography) and visual fields, including peripheral vision. Because of the increased risk among family members, a review of family history is also part of the screening. (Likewise, a positive diagnosis of POAG would be valuable information for close family members.)
quantification of the retinal nerve fiber layer (Optical Coherence Tomography) and visual fields, including peripheral vision. Because of the increased risk among family members, a review of family history is also part of the screening. (Likewise, a positive diagnosis of POAG would be valuable information for close family members.)
Vision lost to glaucoma cannot be restored. The goal with treatment is to slow the disease progress and prevent further vision loss. The most common treatment is a prescription eye drop meant to reduce pressure in the eye. It is important for Dr. Griffith to be aware of other medications you are taking in order to find a compatible treatment for the glaucoma; fortunately there are usually several options. Additional treatment includes laser surgery or sometimes more traditional surgery; both physically alter and improve the drainage structure in the eye. In conclusion, regular eye examinations are vital to prevent unnecessary vision loss. If you are newly diagnosed with POAG or any form of glaucoma, Dr. Griffith can give you more detailed information.