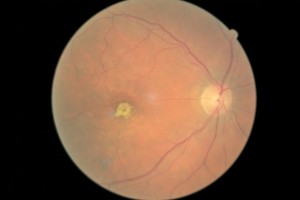
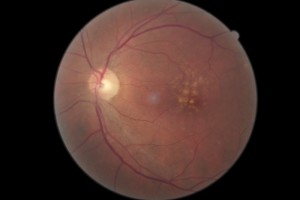
Macular degeneration is a retinal disease which can lead to legal blindness. More specifically, it affects the macula, the portion of the retina important for detailed vision like reading.
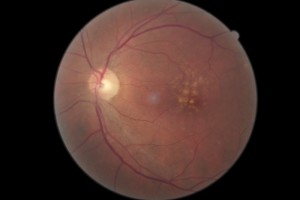
There are two forms of macular degeneration: wet and dry. Dry macular degeneration is usually slower in destruction of the macula, causing gradual to little loss of central vision. The wet form is more aggressive and destroys the central vision faster. The wet form is associated with the presence of abnormal blood vessels growing somewhere within the layers of the retina. These abnormal blood vessels can leak and bleed.
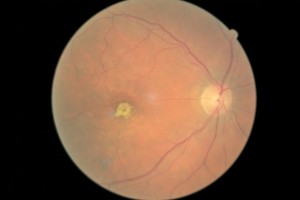
Dry macular degeneration causes a slower loss of tissue. While there is treatment for the wet form, there is no approved treatment for the dry form.
Symptoms of Macular Degeneration include blurry central vision and/or distortion. In some cases, there may be blind spots within the central vision. The vision loss in both types is progressive. It is the rate at which vision loss develops which differentiates the wet form from the dry. Remember, wet macular degeneration causes faster and more devastating loss of vision compared to the dry form.
Treatment for Macular Degeneration
There is no treatment for dry macular degeneration. While AREDS (Age-Related Eye Disease Study) vitamins may be indicated for a small subset of macular degeneration patients, it does not improve the condition or vision. The supplements are primarily preventative. There are different formulations of “eye vitamins,” but the contents of the supplement used for the study were 500 milligrams of vitamin C; 400 International Units of vitamin E; 15 milligrams of beta-carotene (often labeled as equivalent to 25,000 International Units of vitamin A); 80 milligrams of zinc as zinc oxide; and two milligrams of copper as cupric oxide. Copper was added to the AREDS formulations containing zinc to prevent copper deficiency anemia, a condition associated with high levels of zinc intake.
Other preventative measures for both types of macular degeneration include not smoking, regular exercise and a healthy diet.
The mainstay of treatment for wet macular degeneration involves injections into the eye with anti-VEGF (Vascular Endothelial Growth Factor) medications.
These medications (Lucentis, Avastin, Eylea) attach to the abnormal blood vessels, preventing additional leakage and bleeding. Often there can be improvement in vision.
Early treatment is key to maintaining vision. Regular dilated eye examinations are advised.

 A significant amount of other new research is currently aimed at developing therapeutics that treat glaucoma by way of nitric oxide. In fact, the FDA is reviewing at least one new medication that donated nitric oxide. But thanks to this latest study, far fewer people will need it if they load up on their leafy green vegetables before any glaucomatous damage is done.
A significant amount of other new research is currently aimed at developing therapeutics that treat glaucoma by way of nitric oxide. In fact, the FDA is reviewing at least one new medication that donated nitric oxide. But thanks to this latest study, far fewer people will need it if they load up on their leafy green vegetables before any glaucomatous damage is done.



 retinopathy.
retinopathy.