Floaters are spots which can move about in the vision and which are sometimes accompanied by flashes of light. To understand these symptoms it is necessary to understand the basic anatomy of the eye.
Anatomy of the Eye:
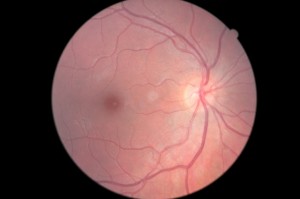
The structure of the eye resembles that of a hollow ball. The 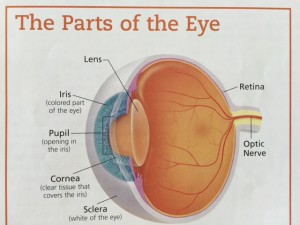 central hollow is filled with a clear jelly called the vitreous. In the front part of this ball there is an opening called the pupil leading to the outside. Looking the inside of the hollow is a thin layer called the retina which is the part of the eye with which a person sees. When we are children the vitreous is solid like cold jello.
central hollow is filled with a clear jelly called the vitreous. In the front part of this ball there is an opening called the pupil leading to the outside. Looking the inside of the hollow is a thin layer called the retina which is the part of the eye with which a person sees. When we are children the vitreous is solid like cold jello.
Floater Formation:
As part of normal changes, the vitreous gel becomes liquefied. This does not occur all at one time so there are pockets of liquefied vitreous next to solid vitreous gel with a filament-like membrane between. When the eye moves the liquid moves easily and sloshes around, causing the filament-like membranes to move and the movement of the membrane casts a moving shadow on the retina which we see as a floater. Where the membranes are attached to the retinal surface, the movement causes a tugging, pulling or traction on the retina. When the retina is pulled or bumped we see the response as a flash of light. Therefore, when the eye moves we see floaters and sometimes we also see light flashes.
If the membrane attached to the retina pulls strongly enough, it can produce a tear or hole in the retina. When a tear forms, there may be a small amount of bleeding, and blood particles moving around in the liquid create floaters which are like a shower of tiny black spots.
Significance of Floaters:
Floaters are not by themselves dangerous, but are a warning that a hole in the retina might exist or that other changes might have taken place. Because of this, it is important for anyone who has recently developed floaters to have a dilated eye examination, including examination of the far edges of the retina where tears are most likely to occur. In the majority of cases this examination will not reveal any holes. If, however, a hole is found in the retina, it usually can be treated with either laser before a more serious problem, such as a retinal detachment, develops.
Light Flashes:
These also can be associated with shrinkage of the gel-like substance (vitreous) as it moves and bumps the retina. Flashes can be caused by rubbing the eyes too hard. Retinal hole formation can also cause light flashes, and so the presence of this symptom requires a careful retinal examination. Flashes can occur from other causes as well.
Follow-up of Floaters and Flashes:
Repeat dilated eye examinations are indicated if suspicious signs are found during an eye examination or if later the patient notices either a sudden increase in floaters and flashes or a veil falling into the vision.
If you are experiencing either new floaters and/or flashes of light, call to have a dilated eye examination sooner than later. Early treatment of holes and retinal tears is less risky and more successful than treatment of a retinal detachment.

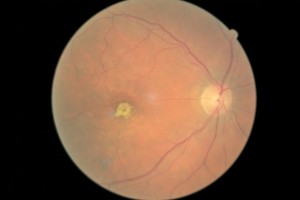
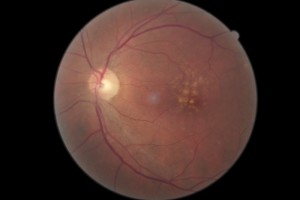
 retinopathy.
retinopathy.